Pain is a complex and multifaceted experience that can significantly affect an individual’s quality of life. It is not merely a physical sensation but also encompasses emotional, psychological, and social dimensions. Chronic pain, in particular, can lead to a cascade of negative outcomes, including anxiety, depression, and social isolation.
Individuals suffering from persistent pain often find themselves unable to engage in daily activities, leading to a diminished sense of self-worth and an overall decline in life satisfaction. The impact of pain extends beyond the individual, affecting relationships with family and friends, as well as workplace productivity. Moreover, the perception of pain is subjective and can vary widely from person to person.
Factors such as cultural background, personal experiences, and psychological state can influence how pain is experienced and expressed. This variability complicates the management of pain, as what works for one individual may not be effective for another. Understanding the intricate relationship between pain and quality of life is crucial for developing effective pain management strategies that address not only the physical aspects of pain but also its emotional and social ramifications.
Key Takeaways
- Pain can have a significant impact on quality of life, affecting physical, emotional, and social well-being.
- Non-pharmacological pain management techniques such as acupuncture, massage, and physical therapy can be effective in reducing pain and improving quality of life.
- Pharmacological pain management options include over-the-counter and prescription medications, which should be used under the guidance of a healthcare professional.
- Integrative approaches to pain management, such as combining traditional and complementary therapies, can provide a holistic approach to addressing pain.
- Mind-body techniques like meditation, deep breathing, and relaxation exercises can help reduce pain and improve overall well-being.
- Lifestyle modifications, including regular exercise, healthy diet, and stress management, can play a significant role in managing chronic pain.
- Supportive therapies such as counseling, support groups, and cognitive behavioral therapy can help individuals cope with the emotional impact of chronic pain.
- Creating a personalized pain management plan that takes into account individual needs, preferences, and goals is essential for effectively managing pain and improving quality of life.
Non-Pharmacological Pain Management Techniques
Non-pharmacological pain management techniques have gained recognition as effective alternatives or complements to traditional medication-based approaches. These methods focus on holistic care, addressing the mind-body connection and promoting overall well-being. Techniques such as physical therapy, acupuncture, and massage therapy have shown promise in alleviating pain and improving function.
Physical therapy, for instance, employs targeted exercises and manual therapies to strengthen muscles, enhance flexibility, and improve mobility, ultimately reducing pain levels. In addition to physical interventions, cognitive-behavioral therapy (CBT) has emerged as a valuable tool in managing pain. CBT helps individuals reframe their thoughts about pain, fostering a more positive mindset and equipping them with coping strategies.
Mindfulness practices, such as meditation and yoga, also play a significant role in non-pharmacological pain management. These practices encourage individuals to focus on the present moment, reducing stress and anxiety that can exacerbate pain. By integrating these techniques into their daily routines, individuals can cultivate resilience against pain and enhance their overall quality of life.
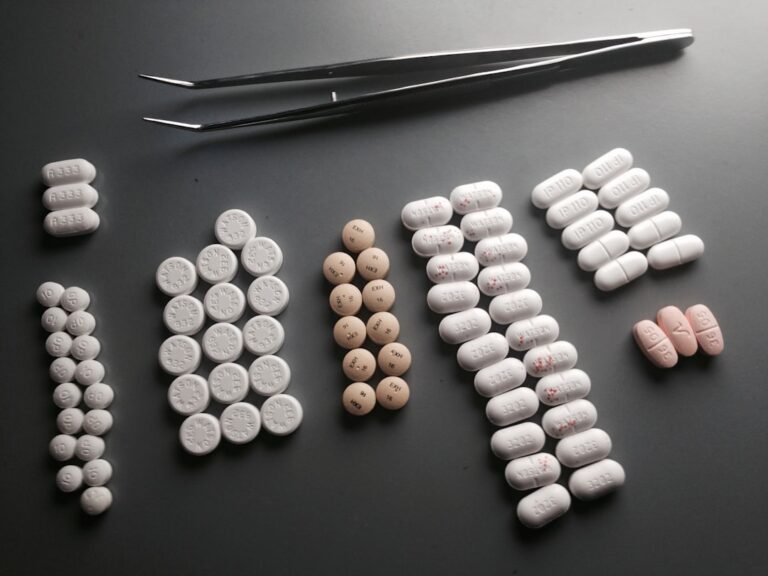
Pharmacological Pain Management Options
Pharmacological options for pain management encompass a wide range of medications designed to alleviate discomfort. Nonsteroidal anti-inflammatory drugs (NSAIDs), acetaminophen, and opioids are among the most commonly prescribed medications for pain relief. NSAIDs work by reducing inflammation and blocking pain signals, making them effective for conditions such as arthritis or muscle injuries.
Acetaminophen is often recommended for mild to moderate pain relief but lacks anti-inflammatory properties. Opioids, while effective for severe pain, pose significant risks due to their potential for addiction and side effects. As a result, healthcare providers are increasingly cautious in prescribing these medications, often reserving them for short-term use or specific cases where other treatments have failed.
Additionally, adjuvant medications such as antidepressants and anticonvulsants have been found to be beneficial in managing certain types of chronic pain, particularly neuropathic pain. The choice of pharmacological intervention should be tailored to the individual’s specific needs and circumstances, taking into account the potential benefits and risks associated with each option.
Integrative Approaches to Pain Management
| Approach | Effectiveness | Side Effects |
|---|---|---|
| Acupuncture | Effective for chronic pain relief | Minimal side effects, such as bruising or soreness |
| Mindfulness Meditation | Reduces pain perception and improves quality of life | No serious side effects reported |
| Yoga | Improves pain, physical function, and mental well-being | May cause muscle soreness or injury if not practiced correctly |
| Cognitive Behavioral Therapy (CBT) | Effective for chronic pain management | No serious side effects reported |
Integrative approaches to pain management combine conventional medical treatments with complementary therapies to create a comprehensive care plan. This holistic perspective recognizes that pain is not solely a physical issue but also involves emotional and psychological components. Integrative approaches may include a combination of pharmacological treatments, physical therapies, nutritional counseling, and alternative modalities such as acupuncture or chiropractic care.
One of the key benefits of integrative approaches is their emphasis on patient-centered care. By considering the individual’s unique circumstances, preferences, and values, healthcare providers can develop personalized treatment plans that address the multifaceted nature of pain. This collaborative approach fosters a sense of empowerment among patients, encouraging them to take an active role in their healing process.
Furthermore, integrative approaches often promote lifestyle changes that can enhance overall health and well-being, ultimately contributing to more effective pain management.
Mind-Body Techniques for Pain Relief
Mind-body techniques have gained traction in recent years as effective methods for managing pain. These practices emphasize the connection between mental processes and physical sensations, highlighting how thoughts and emotions can influence the perception of pain. Techniques such as mindfulness meditation, guided imagery, and biofeedback empower individuals to harness their mental faculties to alleviate discomfort.
Mindfulness meditation encourages individuals to observe their thoughts and feelings without judgment, fostering a sense of acceptance that can reduce anxiety related to pain. Guided imagery involves visualizing calming scenes or experiences to promote relaxation and distract from pain sensations. Biofeedback provides real-time data on physiological functions such as heart rate or muscle tension, enabling individuals to learn how to control these responses consciously.
By incorporating mind-body techniques into their daily routines, individuals can cultivate greater awareness of their bodies and develop effective coping strategies for managing pain.
Lifestyle Modifications for Pain Management
Lifestyle modifications play a crucial role in managing pain effectively. Simple changes in daily habits can lead to significant improvements in overall health and well-being. Regular physical activity is one of the most impactful lifestyle changes individuals can make.
Engaging in low-impact exercises such as walking, swimming, or cycling can help strengthen muscles, improve flexibility, and release endorphins—natural pain relievers produced by the body. Nutrition also plays a vital role in pain management. A balanced diet rich in anti-inflammatory foods—such as fruits, vegetables, whole grains, lean proteins, and healthy fats—can help reduce inflammation and support overall health.
Staying hydrated is equally important; dehydration can exacerbate feelings of fatigue and discomfort. Additionally, prioritizing sleep hygiene by establishing a consistent sleep schedule and creating a restful environment can significantly impact pain perception and overall quality of life.
Supportive Therapies for Chronic Pain
Supportive therapies are essential components of a comprehensive pain management plan for individuals dealing with chronic pain conditions. These therapies aim to provide emotional support, education, and practical strategies for coping with the challenges associated with persistent discomfort. Support groups offer individuals a safe space to share their experiences and connect with others facing similar struggles.
This sense of community can alleviate feelings of isolation and foster resilience. In addition to peer support, professional counseling or therapy can be beneficial for individuals grappling with the emotional toll of chronic pain. Mental health professionals can help individuals develop coping strategies, address underlying psychological issues such as anxiety or depression, and improve overall emotional well-being.
Furthermore, educational resources about chronic pain management empower individuals with knowledge about their conditions and available treatment options. By incorporating supportive therapies into their care plans, individuals can enhance their ability to cope with chronic pain effectively.
Creating a Personalized Pain Management Plan
Creating a personalized pain management plan is essential for addressing the unique needs of each individual experiencing pain. This plan should be developed collaboratively between the patient and their healthcare provider, taking into account various factors such as the type of pain experienced, underlying medical conditions, lifestyle preferences, and personal goals. A comprehensive plan may include a combination of pharmacological treatments, non-pharmacological techniques, lifestyle modifications, and supportive therapies.
Regular follow-up appointments are crucial for assessing the effectiveness of the chosen strategies and making necessary adjustments over time. Pain management is not a one-size-fits-all approach; it requires ongoing evaluation and adaptation based on the individual’s response to treatment. By actively participating in the development of their pain management plan, individuals can feel empowered in their journey toward improved quality of life.
Ultimately, a personalized approach fosters a sense of agency over one’s health and well-being while addressing the multifaceted nature of pain comprehensively.
When it comes to pain management, it is important to consider all available options. One related article that provides valuable insights into this topic is Demystifying Derivatives Law: Essential Concepts for Market Participants. This article delves into the legal aspects of derivatives trading and how market participants can navigate this complex landscape. Understanding the legal framework surrounding financial instruments like derivatives can help individuals make informed decisions when it comes to managing pain and mitigating risks.
FAQs
What is pain management?
Pain management is the medical specialty focused on reducing and controlling pain, whether it is acute or chronic, to improve the patient’s quality of life.
What are the common methods of pain management?
Common methods of pain management include medication, physical therapy, psychological therapy, nerve blocks, acupuncture, and other interventional procedures.
What conditions can be treated with pain management?
Pain management can be used to treat a wide range of conditions, including arthritis, back pain, cancer pain, fibromyalgia, migraines, neuropathic pain, and post-surgical pain, among others.
Who provides pain management services?
Pain management services are provided by a multidisciplinary team of healthcare professionals, including physicians, nurses, physical therapists, psychologists, and pain management specialists.
What are the goals of pain management?
The goals of pain management are to reduce pain, improve physical function, enhance emotional well-being, and minimize the use of opioids and other potentially addictive medications.